Over the past few decades, our understanding of cancer biology has increased rapidly. Yet our ability to translate this knowledge into clinical success remains poor, with reports of eye-wateringly high attrition rates for cancer therapeutics. For example, results published by BIO showed that the likelihood of success from Phase I to FDA approval for cancer treatments was just 5.3%.1 This compares to 23.9% for hematology therapies and 15.5% for metabolic disorders.1
So, where is the oncology field going wrong?
There is growing recognition that the experimental model systems used in many cancer research projects, which include 2D cell cultures, patient-derived xenografts, and genetically engineered murine models, cannot truly recapitulate the cellular heterogeneity of human cancers. They also lack the complex extracellular microenvironment that supports tumor growth, progression, and metastasis. This limits their ability to accurately predict the efficacy, resistance, or toxicity of drug candidates.
Many researchers are looking to advanced 3D models, known as tumor-like organoids or tumoroids, to improve the translational success of preclinical cancer studies. These 3D self-organized cultures are derived from patients’ tumoral tissues, meaning they more accurately represent the diverse genetic, molecular, morphological, and pathophysiological hallmarks of cancer pathology.
Applications for tumoroid models
The excitement surrounding tumoroids stems from their wide range of applications in cancer research: they can be used to study tumor growth, identify novel targeted therapies, and for drug efficacy and toxicity studies. Tumoroids can be co-cultured with immune cells to generate a more biologically relevant representation of the tumor microenvironment. Efforts have also been made to recapitulate the tumor vasculature in tumoroid cultures for a better understanding of angiogenic signaling pathways.
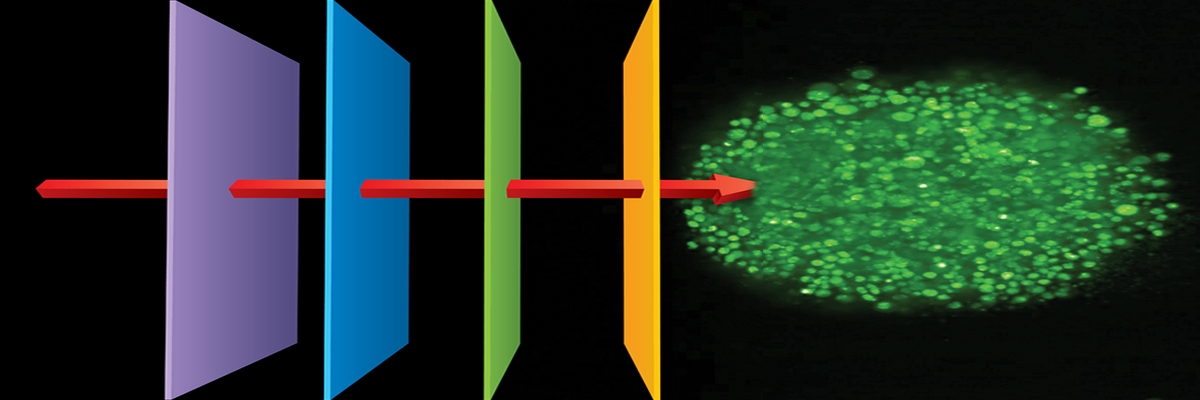
As we embark on an era of precision medicine, tumoroids are being used in combination with high-content imaging for functional drug testing. This involves screening a panel of drugs on patient-derived tumoroids and then imaging and analyzing the phenotypic alterations caused by these compounds. Functional drug testing can be used to help understand patient-specific drug responses and guide personalized treatment.
For example, a team of researchers recently screened over 500 therapeutic bispecific antibodies (bsAb) candidates against a biobank of colorectal cancer tumoroids to assess their functional activity and compare it to organoids derived from healthy mucosa adjacent to the tumor.2 Using high-content image-based screening to capture drug-target interactions the researchers identified one bsAb, MCLA-158, which exhibited therapeutic properties such as growth inhibition, suppression of tumor outgrowth, and inhibition of metastasis initiation. Another group demonstrated how a deep morphological learning approach enhanced their image-based drug screens and successfully identified effective treatment options for patients with advanced blood cancers.3 Studies such as these showcase the potential of functional screening to advance precision research and fill the gap between conventional screening approaches and clinical success.
Limitations to the widescale use of tumoroids
While there are numerous advantages to using tumoroids over traditional cancer models, several challenges and bottlenecks remain. First, the cost of establishing and maintaining tumoroids is often high, with success rates varying between cancer types. Second, the field is relatively new and lacks optimized and standardized culture and co-culture conditions, bioanalytical processes, and quality control measures. Establishing validated procedures will help improve reproducibility and facilitate its wider use in high-throughput screens. It will also help with regulatory processes and speed up approvals. Despite these challenges, tumoroids are adding another dimension to the oncology field and represent an exciting opportunity to help replace, reduce, and refine (3Rs) the use of animals in cancer research.
Revvity Inc. does not endorse or make recommendations with respect to research, medication, or treatments. All information presented is for informational purposes only and is not intended as medical advice. For country specific recommendations, please consult your local health care professionals.
References:
- Clinical Development Success Rates and Contributing Factors 2011–2020. BIO; 2021 Feb [cited 2022 Nov]. Available from: https://www.bio.org/clinical-development-success-rates-and-contributing-factors-2011-2020
- Herpers B, Eppink B, James MI, Cortina C, Cañellas-Socias A, Boj SF, et al. Functional patient-derived organoid screenings identify MCLA-158 as a therapeutic EGFR × LGR5 bispecific antibody with efficacy in epithelial tumors. Nature Cancer. 2022Apr;3(4):418–36.
- Heinemann T, Kornauth C, Severin Y, Vladimer GI, Pemovska T, Hadzijusufovic E, et al. Deep morphology learning enhances ex vivo drug profiling-based precision medicine. Blood Cancer Discovery. 2022Nov;3(6):502–15.